Peripheral Procedures
Diagnostic Peripheral Angiogram
 A peripheral angiogram is an x-ray imaging test used to view the blood vessels in the pelvis, legs, knees, ankles and also, less commonly, the arms, neck and even brain. Specialists often use this test to study narrow, blocked, enlarged or malformed arteries and veins in many areas of the body.
A peripheral angiogram is an x-ray imaging test used to view the blood vessels in the pelvis, legs, knees, ankles and also, less commonly, the arms, neck and even brain. Specialists often use this test to study narrow, blocked, enlarged or malformed arteries and veins in many areas of the body.
A peripheral angiogram is used to diagnose a variety of conditions, including:
- blockages of the arteries, called Peripheral Artery Disease (PAD);
- malformed arteries, known as vascular malformations;
Indications for an angiogram are;
- claudication that is lifestyle limiting
- rest pain
- non healing ulcer
- ultrasound evidence of flow limiting lesion
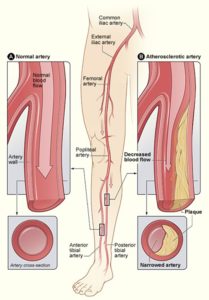
Peripheral Artery Disease (PAD)
Peripheral artery disease, or PAD, refers to arterial disease that occurs outside of the heart or brain. In PAD, the arteries that carry oxygenated blood throughout the body become narrowed or even blocked, usually as a result of atherosclerosis, or plaque. As plaque growth progresses, clots may develop and completely block the artery. This can lead to organ damage and loss of fingers, toes, or limbs, if left untreated. PAD most commonly affects the arteries in the legs, but it also can involve arteries that carry blood to the head, arms, kidneys and gastrointestinal (GI) tract.
Many people with PAD have mild or no symptoms. Those that do often mistake them for something else, such as a back or muscle problem. Symptoms include a tight, aching or squeezing pain in the calf, thigh or buttock. This pain usually happens after you have walked a certain distance, ie after you have walked 100m or 200m. The pain goes away if you stop walking. As PAD gets worse you may experience leg or foot pain at rest, or pain that remains even after you have stopped \walking. You may also experience cold or numb toes or have sores / ulcers that are slow to heal.
Among the risk factors for PAD are diabetes, smoking, high cholesterol and high blood pressure. Most cases occur in people older than 50.
Vascular ultrasound, Doppler ultrasound, catheter angiography, CT angiography (CTA), or MR angiography (MRA) may be used to help evaluate your condition.
Lifestyle changes such as dietary modifications, exercise and smoking cessation often are the first choices for patients with early-stage PAD. Bypass surgery or interventional procedures such as angioplasty, catheter-directed thrombolysis or atherectomy may be used to help improve blood flow.
Angioplasty – Treatment
Your specialist will refer you for an Imaging test to assess the arteries of the lower limb, such as an Ultrasound. If this shows narrowing’s that can be treated with an Angioplasty, they will refer you for a Peripheral Arteriogram (Angiogram), see “Angiogram” for more information.
Once your peripheral angiogram has been carried out and a diseased vessel has been identified, the doctor will usually proceed to treat the diseased area at the same time. This is referred to as percutaneous transluminal angioplasty (PTA) or intervention. If you do require angioplasty, it will be done through the same tube that has been placed in your groin for the angiogram:
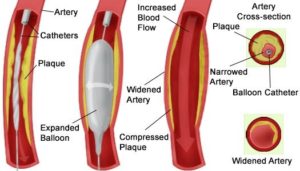
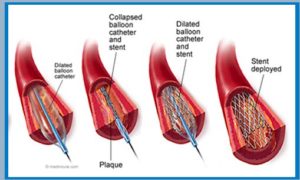
Angioplasty, with or without vascular stenting, is a minimally invasive procedure. It is used to improve blood flow when a vein or artery is too narrow or blocked. It is usually done in an interventional radiology suite rather than operating room.
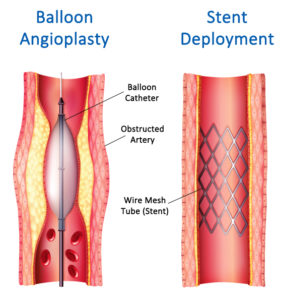
In angioplasty, using x-ray guidance, the doctor crosses the narrowing or blockage with a guide wire. This allows the balloon-tipped catheter to pass over the wire. Once across the blockage, the balloon will be inflated for a short time. Sometimes the balloon needs to be inflated more than once. Or, other blood vessels need to be treated during the same procedure. More x-rays are taken to see how much blood flow has improved. If the narrowing or blockage does not respond to balloon treatment, you specialist may consider placing a stent in the narrowing. A stent is a small expandable mesh tube made from a special metal alloy. Once positioned at the point of narrowing, the stent is opened to a predetermined width to hold the narrowed artery open. A stent is only inserted where there is likelihood that the balloon angioplasty will not remain patent.
Once the doctor is satisfied with the result, catheter, wire, and sheath will be removed and pressure is applied to stop any bleeding. Sometimes, your doctor may use a closure device to seal the small hole in the artery. This will allow you to move around more quickly. No stitches are visible on the skin.
You may need to lie in bed with your legs straight for several hours post procedure.
What are the Limitations of Angioplasty and Vascular Stenting?
Angioplasty with vascular stenting is just one way to treat narrowed or blocked arteries. Medication and exercise are often the first step.
Angioplasty does not reverse or cure the underlying disease of atherosclerosis. It is very important for patients to make lifestyle changes, including eating a healthy diet that is low in saturated fat, exercising and not smoking. Patients with diabetes, high blood pressure and/or high cholesterol need to follow the treatment plan prescribed by their doctors.
Angioplasty may have to be repeated if the same artery becomes blocked again, a condition called restenosis. If a stent is placed, the chance of restenosis is reduced but it can still occur.
Angioplasty and vascular stenting for peripheral artery disease (PAD) affecting arteries in the pelvis and legs is less successful when multiple leg vessels are narrowed or when small vessels have to be opened.
This visit may include a physical check-up, imaging exam(s) and blood tests. During your follow-up visit, tell your doctor about any side effects or changes you have noticed.
Endovascular Aneurysm Repair – EVAR
EVAR is a minimally invasive procedure performed as an alternative to surgery, to repair an abdominal aortic aneurysm (AAA).
What is an Abdominal Aortic Aneurysm, (AAA)?
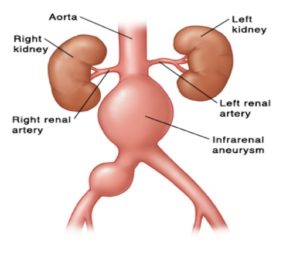
The aorta is the largest artery in the body. It transports oxygenated blood away from the heart to all parts of the body. It runs from the heart through the chest, where it is called the Thoracic Aorta. The portion of artery which lies deep inside the abdomen is called the abdominal aorta, this supplies blood to the lower part of the body.
The normal diameter of the abdominal aorta is about 2cm. If the wall weakens or stretches, then the pressure of blood flowing through it can cause this area to expand or bulge outwards. This is called and Abdominal Aortic Aneurysm (AAA). An aneurysm occurs if the arterial wall weakens and develops a bulge, meaning blood is flowing to the weakened area.
Indications for Treatment.
AAA develops slowly over time and the exact causes of the degenerative process remain unclear. Most aneurysms cause no noticeable symptoms, although occasionally they cause pain in the abdomen or pain in the chest, lower back (due to pressure on surrounding tissues) or in the legs (due to disturbed blood flow).
If the aneurysm is over 5.5cm, we would start considering treatment because the risk of rupture increases above this size. Should an aneurysm expand rapidly, tear, or leak, the following symptoms may develop suddenly:
- intense and persistent abdominal or back pain that may radiate to the buttocks and legs
- sweating and clamminess
- dizziness
- nausea and vomiting
- rapid heart rate
- shortness of breath
Treatment for AAA:
-
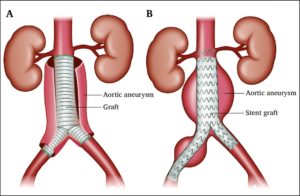
Surgical method (Open Repair)
This involves a surgical incision into the abdomen to expose the abdominal aorta and the aneurysm. The aorta is clamped above and below the aneurysm. The aneurysm is cut open and a synthetic tube (graft) is sewn (sutured) into place across the aneurysm which is attached at the top and bottom to a normal section of aorta. The wall of the aneurysmal aorta is wrapped around the graft and sewn into place. This procedure is done in an operating theatre under general anaesthesia.
-
Endovascular Repair EVAR
This is the placement of a stent-graft (fabric-covered tube) into the aneurysm through a small incision in each groin area to access the femoral artery. On occasions, the procedure may be performed entirely through the skin (percutaneous) without any incision.
Using X-ray control and injecting contrast media, the doctor will visualize the aneurysm and plan the endovascular repair. Using specialised endovascular equipment and X-ray guidance, a stent-graft (in a collapsed position) is inserted through the femoral artery and advanced up into the aorta to the site of the aneurysm.
Once in the required position, the stent graft is expanded. The graft material will bond with your arterial wall and blood will flow through the stent instead of the weakened aneurysm. Using X-ray imaging, the doctor checks the position of the stent graft and ensures there are no leaks. Following this, the instruments are removed.
This procedure often takes around two hours but depending on your individual circumstances, it may be shorter or longer than this. It is conducted in an angiography suite usually under general anaesthesia. It is conducted by an interventional radiologist, vascular surgeon and anaesthetist, who will be assisted by nurses and other highly trained staff.
The benefit of the endovascular approach is reduced recovery time, particularly as there are no large incisions that need to heal. Patients are usually discharged 5 to 7 days after open repair and 1 to 2 days after endovascular repair.
You may be suitable for elective EVAR if your aneurysm is large enough (5.5cm wide or more) and you have a long enough area of normal artery for the stent graft to attach to securely.
Potential complications include:
- Leaking of blood around the graft (endoleak)
- Movement of the graft away from the its optimal location (“migration”, uncommon)
- Blockage of blood flow through the graft (uncommon)
- Reduced blood flow to the bowel and / or kidneys
- Vessel problems, rupture, dissection.
Endoleaks:
Stent grafts can sometimes leak blood through the areas where the graft components join, or they can allow blood to leak back into the aneurysm sac through small arteries feeding the sac. These leaks are called “Endoleaks”. Some of these leaks stop by themselves, but others need to be treated. These leaks can occur years after the procedure and can be dangerous if the aneurysm continues to enlarge. Thus, after the EVAR procedure specialists require patients to have regular surveillance checks, usually via an ultrasound scan.
Vascular Embolisation
This is a non-surgical, minimally invasive procedure that blocks one or more blood vessels or abnormal vascular channels.
In a catheter embolization procedure, medications or synthetic materials called embolic agents are placed through a catheter into a blood vessel to prevent blood flow to the area.
This is done by introducing medications or synthetic materials called embolic agents, through a catheter into a blood vessel to block blood flow to an area of the body. It may be used to close off vessels supplying blood to a tumour or to eliminate abnormal connections between arteries and veins
Your physician will select an embolic agent depending on the size of the blood vessel or malformation and whether the treatment is intended to be permanent or temporary. These include:
- Gelfoam™, a gelatin sponge material, which is cut into small pieces that are injected into an artery and float downstream until they can go no further. After a period ranging from a few days to two weeks, the material dissolves. Gelfoam is used to control bleeding until the cause can be identified and fixed, or until it has time to heal on its own.
- particulate agents, including Polyvinyl alcohol (PVA) and gelatin-impregnated acrylic polymer spheres, which are suspended in liquid and injected into the bloodstream to block small vessels. These agents are used to block, or occlude, vessels permanently.
- various sized metal coils made of stainless steel or platinum are used to block large arteries.
- liquid sclerosing agents, which are used to destroy blood vessels and vessel malformations. Filling a vessel or a vessel malformation such as a fistula with this liquid agent causes blood clots to form, closing the abnormal vascular channels.
- liquid glue, which can be inserted into a fistula or arteriovenous malformation (AVM) where it hardens, filling in this unnecessary passageway between artery and vein.
Embolisation is used to treat a wide variety of conditions affecting different parts of the body.
- Uterine Fibroids
- Ovarian Veins
- Varicocele Embolisation
- Prior to tumour resection (to reduce blood flow in affected area prior to surgery)
- Vascular malformations, A-V malformations – (abnormal connection or connections between arteries and veins). These passageways, which may occur anywhere in the body including the brain or spinal cord, act like a short circuit to prevent blood from fully circulating and delivering oxygen where it is needed.
- Decrease the size of congenital venous malformations (a tangle of veins that did not develop into a normal straight vein) in order to decrease pain, swelling and clot formation.
How does the procedure work?
Using x-ray imaging and a contrast material to visualize the blood vessel, the interventional radiologist inserts a catheter through the skin into a blood vessel and advances it to the treatment site. A synthetic material or medication called an embolic agent is then inserted through the catheter and positioned within the blood vessel or malformation where it will remain permanently. Some patients may require a general anaesthetic, but most times just using local anaesthetic and pain relief if necessary.
Arteriovenous Malformation (AVM)
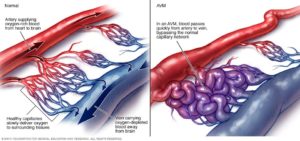
An arteriovenous malformation (AVM) is an abnormal tangle of blood vessels connecting arteries and veins which disrupts normal blood flow and oxygen circulation.
An arteriovenous malformation can develop anywhere in your body but occurs most often in the brain, neck and spine, but they are also found in the arms, legs, lungs, liver an reproductive system.
AVMs cause blood to bypass the capillaries, the smallest blood vessels, and pass directly from the arteries to the veins. Some AVMs cause no problems. Others may eventually burst and bleed causing serious problems.
When an AVM disrupts this critical process, the surrounding tissues may not get enough oxygen, and the affected arteries and veins can weaken and rupture.
The cause of AVMs is not clear. They’re rarely passed down among families.
Treatment:
One method of treatment is embolisation. This is much less invasive than surgery. The procedure involves using a thin plastic tube inserted into an artery. The doctor will use x-ray guidance and contrast media injections, to manoeuvre the catheter tip to the site of the AVM. A special type of liquid, metallic coils or other embolic substance is then placed or released to stop the blood flow to the AVM. This approach may require a series of treatments. Some AVMs may be embolised prior to surgical removal.
After treatment you may need follow-up imaging to make sure the AVM is completely removed or destroyed. There is still a risk of bleeding if some of the AVM remains after embolisation treatment.
Arteriovenous Fistula Malformation.
An abnormal connection between an artery and vein, often due to trauma. Small AV fistulas that occur in your legs, arms, lungs, kidneys or brain often occur without any symptoms and only need to be monitored by your doctor. Larger AV fistulas may cause:
- Swelling along with a reddish appearance on the skin surface
- Purplish, bulging veins that you can see through your skin, similar to varicose veins
- Swelling in the arms or legs
Regardless of the cause, serious complications can develop if a large AV fistula is not treated.
AV fistula can be treated with catheter embolisation in a procedure similar to that previously described.
Upper Limb Venography
A venogram is a special x-ray examination of the veins in your arm using x-ray contrast medium, which when injected into a vein makes them show up better on x-rays. Upper extremity venography allows your doctor to look for blockages, blood clots, or vascular abnormalities in the veins in your neck and arms.
In a venogram procedure, an interventional radiologist uses an x-ray camera called a Fluoroscopy to inject contrast into the veins to see the blood flow in order to determine the condition of the veins.
The nurse or doctor, will insert a luer (plastic needle) into a vein to inject the contrast agent As the contrast material flows through the veins being examined, several x-rays are taken. Your arm will be moved into different positions so that the x-rays can be taken to check whether your vein is being pinched at any point in your upper chest area.
This examination is usually done on an outpatient basis, and takes around 30-45 minutes.
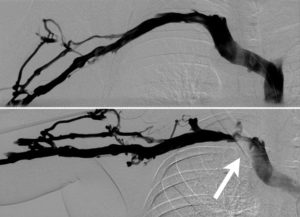
Top image: arm in neutral position.
Bottom image: obtained during abduction of the arm showing the venous thoracic outlet syndrome with stenosis (narrowing) of the subclavian vein, (white arrow).
IVC FILTER PLACEMENT
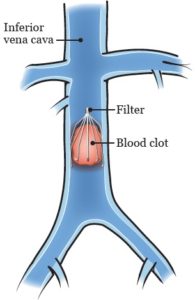
The inferior vena cava is the largest vein in your body. It carries blood from your lower body to your heart and lungs. An IVC filter is placed just below your Renal Veins to prevent any blood clots reaching your lungs and causing Pulmonary Emboli (PE) and consequently shortness of breath.
Blood clots are treated with blood thinners but some people may not be able to receive this treatment. In those cases, an IVC filter may be placed. If a blood clot develops in a vein below your heart and blocks your normal blood flow it usually causes swelling, redness, and pain in the area.
Your IVC filter will be placed by an interventional radiologist (a doctor who specializes in image-guided procedures). A tube, through which the filter will be passed, will be placed into a vein in your groin or neck and guided into the IVC in your abdomen using fluoroscopy (a type of x-ray) to visualize the guiding of the tube (sheath) into your IVC. X-ray dye will be injected through the sheath and images will be taken of the IVC in your abdomen that connects your leg veins to your heart. Next, the filter will be positioned and released where it attaches itself to the wall and remains in place. It will filter your blood, trapping any pieces of a clot as they flow from your legs.
Once the filter is placed, the sheath will be removed and pressure will be applied over the site where it went into the skin for about 5 minutes. When the bleeding has stopped, a bandage will be placed over the site.
Your doctor will explain the procedure and answer any questions you have. They will also ask you to sign a consent form (a form that says you agree to the procedure and understand the risks).
What Are the IVC Filter Types We Offer?
There are two types of filters (permanent and retrievable) that can be placed in your body. Your doctor will determine which filter is right for you.
-
Permanent Filters
Permanent IVC filters are placed in patients including, but not limited to, those that are unable to take anticoagulant medications or patients that are elderly. These IVC filters are permanently left in place in your body.
-
Retrievable Filters
Retrievable filters are placed and then can be removed once your risk for clotting has been decreased. Retrievable filters are placed in patients that have only a temporary risk of Pulmonary Embolism (PE), need to hold their anticoagulation medications for surgery or have temporary bleeding problems. A retrievable filter can always be left in place permanently if your doctor decides this is best for you or it can be removed at a later date when your doctor determines it is safe to do so.
How Is an IVC Filter Removed?
If you have a temporary filter and your physician has determined it is no longer necessary, the filter can be removed in a procedure similar to the way in which it was placed. X-ray dye (contrast) will be injected around the IVC filter to verify that the area beneath the filter is free of blood clots and that it is safe to proceed with removal. A catheter-based snare will be used to engage the hook at the end of the filter and the filter will then be enveloped by a removal sheath and removed from your body.
Why perform it?
There are a number of treatments available to manage or prevent pulmonary emboli and DVT, including conservative (medical) therapy, IVC filters, intravenous systemic thrombolysis, catheter thrombolysis and a surgical operation.
Your suitability for this treatment depends on a number of factors, including how stable your blood pressure is and how well your heart is working. Other factors which will be taken into consideration are the type of IVC filter and your clinical situation, as permanent placement means you will need to take medication to prevent blood clotting for the rest of your life.
What are some common uses of the procedure?
Inferior vena cava (IVC) filters are placed in patients who have a history of or are at risk of developing blood clots in the legs, including patients:
- diagnosed with deep vein thrombosis (DVT).
- with pulmonary embolus.
- who are trauma victims.
- who are immobile.
What are the benefits vs. risks?
Benefits
- No surgical incision is necessary—only a small nick in the skin that does not need stitches.
- The filter has a high rate of success in protecting lungs from serious pulmonary embolus (PE) in patients who have failed conventional medical therapy or cannot be given conventional medical therapy.
Risks
- Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
- There is a very slight risk of an allergic reaction if contrast material is injected.
- Any procedure that places a catheter inside a blood vessel carries certain risks. These risks include damage to the blood vessel, bruising or bleeding at the puncture site, and infection. The doctor will take precautions to mitigate these risks.
- There is a chance that the IVC filter can lodge in the wrong place, change position or penetrate through the vein (which can rarely lead to injury of a nearby organ).
- The IVC filter or a piece of the IVC filter may break loose and travel to the heart or lungs causing injury or death.
- Rarely, IVC filers become so filled with clots that they block all flow in the blood vessel, causing swelling in the legs.
- In some cases, retrievable filters become scarred to the vein and cannot be removed, in which case they are left in permanently (as they are also designed to do).
Call your doctor right away if you have any of the following post procedure:
- Coldness or numbness in one of your limbs
- Bleeding at the site that doesn’t stop with pressure
- Swelling or pain at the incision site that gets worse
- Fluid leaking from the incision site
- Redness or warmth at the incision site
- Fever
- Chest pain
- Headache or nausea that don’t go away
Follow all of your doctor’s instructions. This includes any advice about medications, exercise, and wound care. Your doctor may prescribe blood thinner medication to help prevent blood clots.